

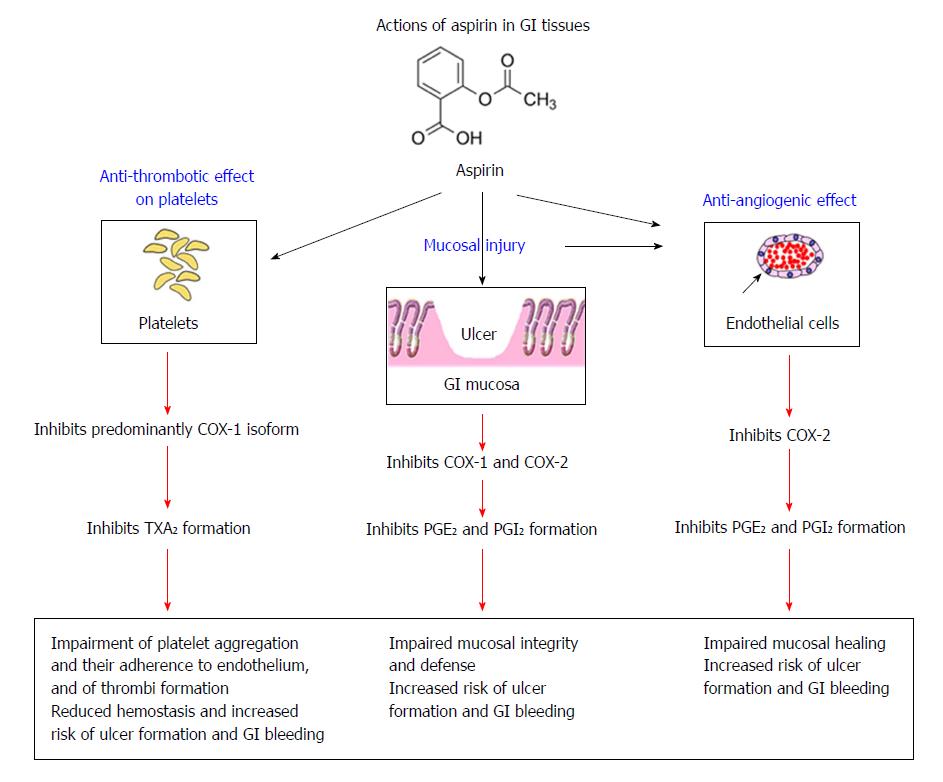
Hypertension poses the particular hazard of intracranial haemorrhage (ICH) with an incremental risk beginning at systolic pressure >160 to 170 mmHg. Important risk factors for bleeding have been identified in several clinical trials. There is heterogeneity in the definition of bleeding, and commonly used classifications include TIMI, BARC, GUSTO, PLATO, GRACE, etc. On the other hand, primary percutaneous coronary intervention (PCI) resulted in infrequent major bleeds (1.6%) in a large, prospective study. In general, fibrinolysis causes 0.9-1% of intracranial bleeds and 4-13% of major non-cerebral bleeds (defined either as those requiring blood transfusion or as those that are life-threatening). Therefore, caution must be exercised to prevent bleeding complications, although urgent reperfusion/antithrombotic strategies are life-saving in STEMI. Gastrointestinal and intracranial bleedings carry a worse prognosis. Despite diverse definitions in clinical trials, bleeding is also known to increase the rates of recurrent MI and stroke, and results in a longer hospital stay. Blood transfusions in this setting are known to result in higher mortality.
There seems to be a linear association between bleeding and death in patients with STEMI, regardless of the success or failure of reperfusion therapy. Successful treatment of STEMI is often offset by the resultant bleeding events.


 0 kommentar(er)
0 kommentar(er)
